Let’s simplify + unify the healthcare payments experience together
It’s going to take a collaborative effort to solve the greatest challenges in the revenue cycle, and exceed the needs of providers and patients. And when there is an opportunity to combine great technologies through integration, great outcomes can be achieved. We’re excited to offer a suite of revenue cycle APIs to help achieve the ultimate experience.
We believe in the quintuple win – a win for the provider, a win for you, a win for us, a win for your developers, and most importantly, a win for patients.
So whether you are a developer at a provider, start-up, established health IT application, a technology backed services provider to healthcare, or payer wanting to improve the patient experience, we want to hear from you.
Come take a look at our Revenue Cycle integration capabilities.
Fast & seamless integration
Transform your revenue cycle with ease. Whatever your existing systems, our cost-effective technology is compatible with all of them and gets up and running quickly. Give your staff the intuitive solutions that will make their jobs easier and their workflows more efficient.
Technologies and API’s available:
REST APIs, web services, sFTP, HL7, batch, X12 EDI, RPA (bot)

Integration Basics
Waystar offers several APIs and integration options for most of our product lines. We are constantly working to add new integration capabilities and build out additional capabilities to make our award-winning RCM capabilities available to you in your applications.
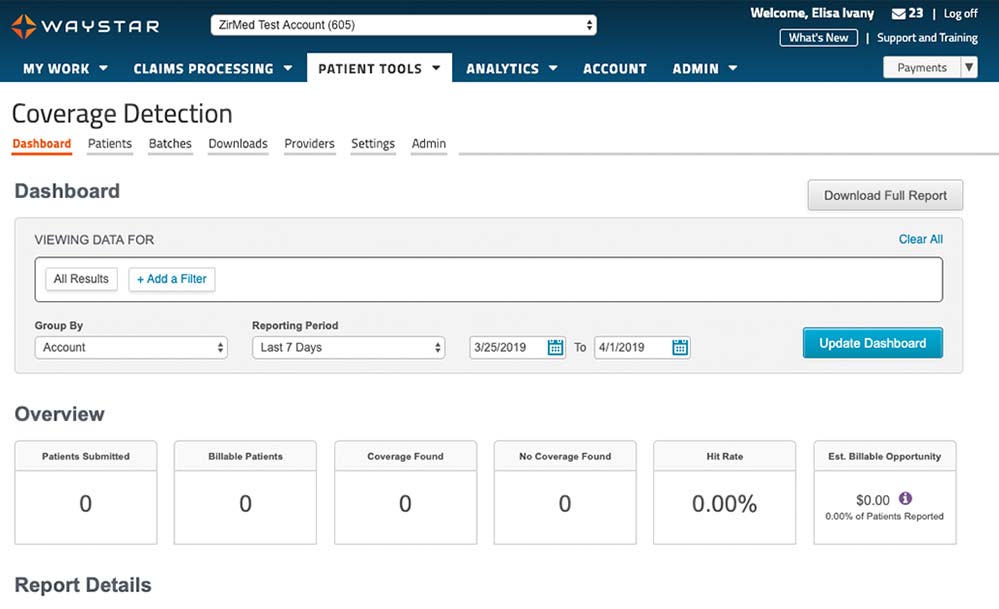
Financial Clearance
Our platform draws on the latest technology and predictive analytics to simplify eligibility verification and prior authorization processes, help patients understand their financial responsibility, give providers visibility into patient propensity to pay and more. With Waystar, you can bring in more revenue up front and provide a more transparent, positive experience for patients.
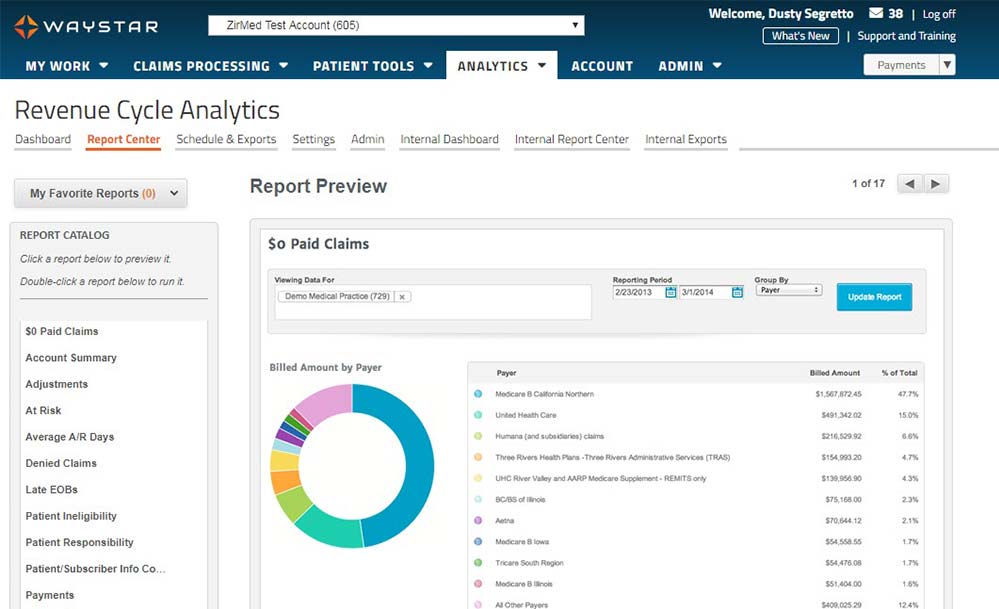
Revenue Capture
Between missing charges, coding mistakes and DRG underpayments, many healthcare organizations are losing out on a significant amount of revenue they’re owed. Powered by predictive analytics and machine learning—and supported by a dedicated team of certified coding experts—our suite of Revenue Capture solutions can help you identify and correct these errors. With Waystar, your team can easily recover more revenue and save hours of work.
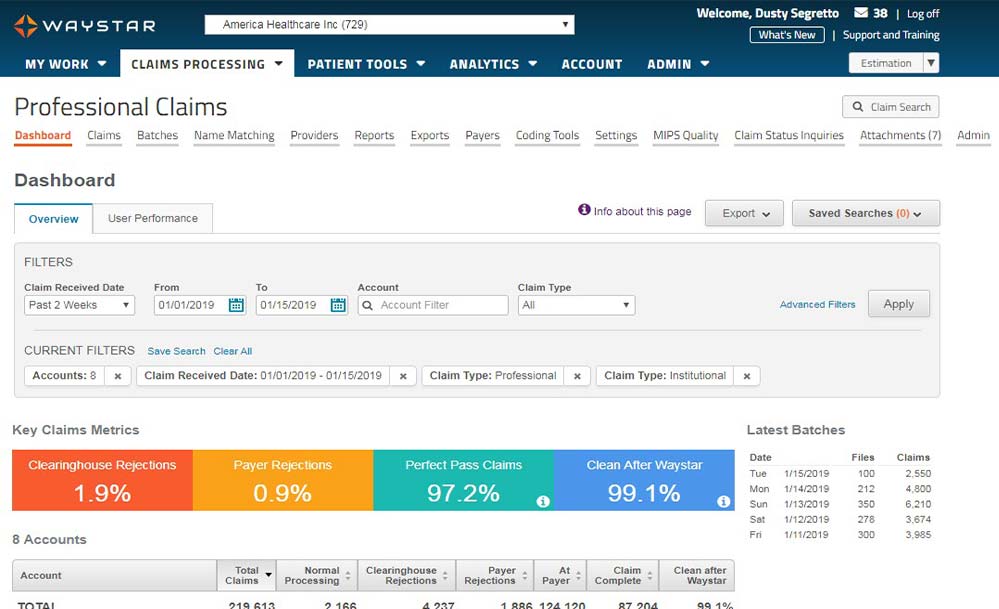
Claim Management
Submitting a clean claim to payers the first time can be a challenge. What’s even worse are lost claims … and lost revenue. Waystar’s Claims Management solution can help you effortlessly capture those missing revenues.
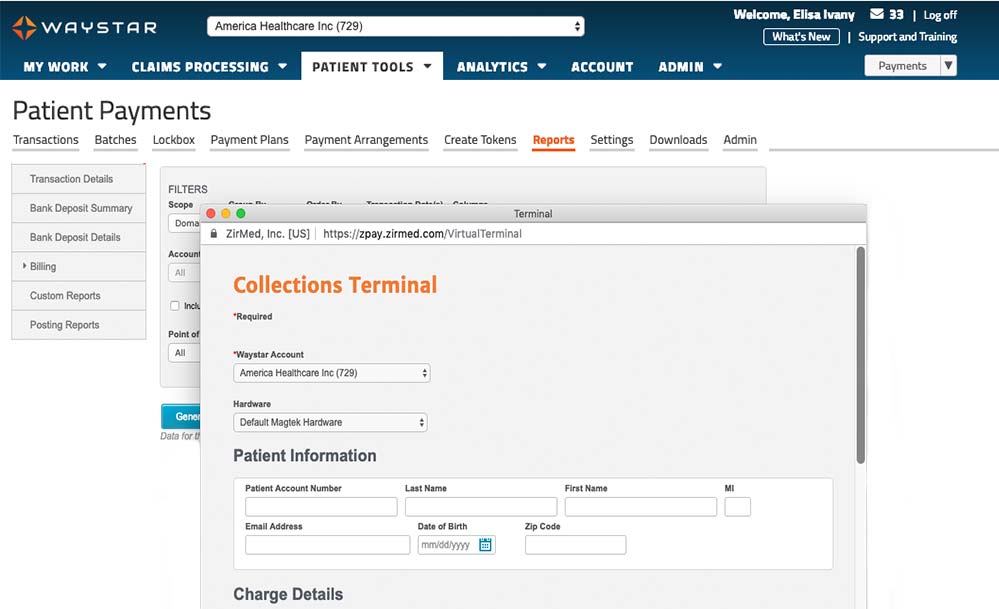
Payment Management
The processes of paying for healthcare can be stressful for providers and patients alike. With Waystar, you can give your team the solutions they need to maximize payment from both patients and payers. You can also provide a more transparent and positive financial experience for patients. Explore our reimbursement suites and find out how much easier collecting payment can be.
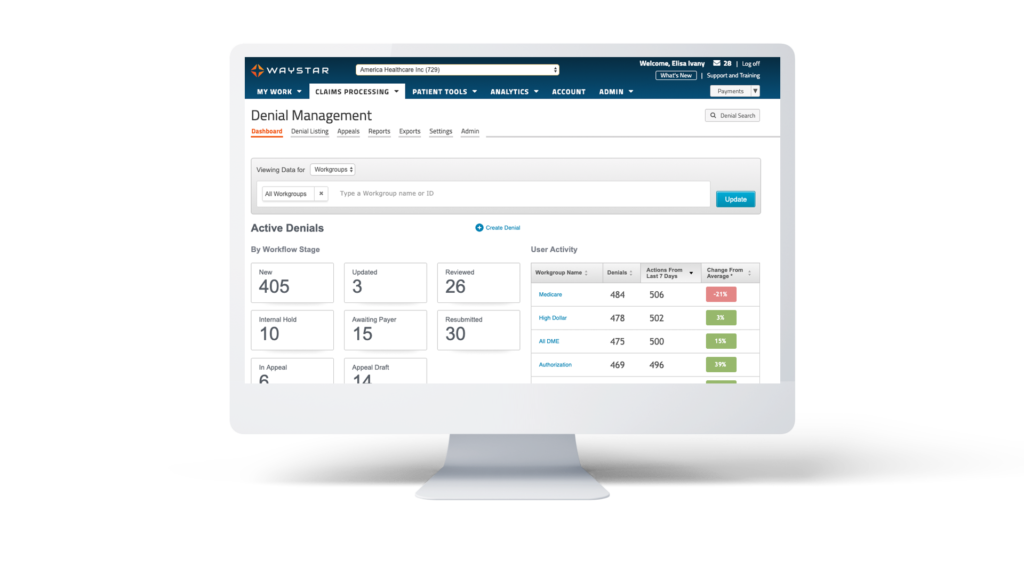
Denial Prevention & Recovery
Outdated denial processing and high workload mean you’re probably leaving a lot of revenue on the table. Waystar’s Denial Prevention + Recovery suite helps you manage, appeal and even prevent denials to ensure that less revenue slips through the cracks.
